Quality health care is not a cheap pleasure. To provide citizens with maximum access to the medical services, the developed countries facing the challenge of an ageing population are paying increasing attention to nursing services. According to international best practice, giving broader credentials to nurses makes it possible not only to expand access to health services but also to enhance their quality. At the same time, Ukraine’s medical reform has left nursing personnel on the sidelines. And this is already having negative effects.
During the COVID-19 pandemic in 2021, the former Vesele ATC (Luhansk region) was left without access to non-emergency health care. When the only family doctor available there quit his job, it automatically led to abolishing the local ambulatory care clinic and feldsher-midwife stations because according to current regulations “An FMS is supervised by a doctor, with whom the residents of the settlement(s) signed the declaration”, and it cannot work without her/him.
The issue of access to health services could be solved by empowering nurses, e.g. enabling them to examine patients or prescribe basic medicines. But Ukraine has just taken the first step in that direction, offering different educational levels for nurses. As of 2008, nurses can get a master’s degree, and as of 2019, they can receive a doctorate and engage in research.
According to the director of a higher education institution in the field of nursing, “a nurse with a bachelor’s or master’s degree can [replace a doctor in an FMS or an outpatient clinic in a village]. If the ambulant clinic indeed has the necessary equipment, and she is appropriately trained. And, probably, it’s still necessary to receive specialty training”.
This article is based on the analytical report “Invisible Nursing: How to Change the Situation? A Roadmap for the Development of Nursing in Ukraine for 2021-2023” prepared under the project “Creation of the Roadmap for nursing development in Ukraine” provided with the support of the International Renaissance Foundation. The project is implemented by the analytical platform Vox Ukraine and the Center for Nursing Development of the Ministry of Health of Ukraine.
However, in the labor market, nurses are still seen only as “doctor’s hands“. The nurse’s duties include participating in the treatment and diagnostic process, implementing the appointments and the doctor’s instructions, and paperwork. As well as an expected – but formally not prescribed – ability to understand the doctor “at a glance”. This gives nurses a sense of inferiority in their professional field cementing the status quo. Due to the previously existing position of chief physician managing the hospital, doctors are the ones who have a say in medical institutions today. Therefore, despite the legal possibility to influence the terms of collective agreements, the de facto situation remains the same, with most nurses continuing to receive a minimum wage regardless of the scope of or specific tasks they perform. Low wages force nurses to work additional jobs, which leads to work overload and a lower quality of work.
“I’m not happy with only one thing – the nurses’ inappropriate pay package and the fact that the state implemented this reform. Many nurses were laid off, that is, they’d calculated that one nurse could do the work of two or three nurses in the ward. If, at least, they were paid decently, then maybe the girls would keep working, but if their salary is the same, and there’s plenty of work… And you know, when a nurse is overwhelmed with work, the quality of that work goes down,” a nurse said.
This is a worrying trend because successful implementation and perception of health care reform in Ukraine largely depend on the ability of nurses to attend and provide care to patients on an outpatient basis, in a hospital or at home.
With the large-scale reform changing the principles of funding medical institutions that began in late 2017 with the adoption of the Law On Financial Guarantees for the Provision of Medical Services, the change agents overlooked the role and functions of nurses. There is no separate package of medical services to be funded by the National Health Service of Ukraine (NHSU). Therefore, although they are the ones ensuring the implementation of а large part of the tasks including of a family doctor (e.g. preventing disease, promoting a healthy lifestyle, carrying out vaccinations), no one talks about their contribution, nor is it separately funded. So the nurses’ moral and financial dependence on doctors has not been reduced. Even the Fundamentals of the Laws of Ukraine on Health Care describe the roles of doctors but never mention the functions of nurse staff at the primary, secondary and tertiary levels of health care.
“If the doctor examined a patient and instructed the nurse to perform the procedures, and then the nurse performs them herself… If it was only under the doctor, the doctor would get all the money, and how much money he’ll distribute to the nurse isn’t known. But in this case, the doctor performed his function and the nurse performed hers,” a doctor said.
And how is it in the world?
In developed countries, nurses are given greater independence, and their work is overseen through separate licensing.
For instance, in the UK, nurses have separate regulators and a trade union. Upon graduation, they are automatically entered into the nurse and midwife register (foreigners need to pass a separate exam). Being registered there requires paying a membership fee. Only those in the register are allowed to work in the UK. Over the last few decades, the nurses have taken on many new functions. Specifically, without the participation of doctors, nurses can now provide treatment services that do not require medical intervention, prescribe patients a full list of medicines and even do blood transfusions. The British medical system aims to provide as many services as possible in people’s homes since it makes it possible to avoid cross-contamination of patients and reduces the risk of infection with resistant nosocomial strains. Community nurses provide the bulk of such services. Private nursing practice is allowed in the UK, but not very common. It is found mainly in the aesthetics industry (cosmetic medicine, Botox injections, etc.) and midwife services.
The situation is similar in the United States. To obtain a license to work in a particular state, nurse must meet the requirements of the local regulator and pass the exam (NCLEX). In the United States, nurses provide basic care to patients during the night and therapeutic care during the day. All radiologists, specialists in ultrasounds and diagnosticians of other specialties have received nursing education and provide their conclusions without the participation of a doctor. In some states, anesthesia for simple surgeries is provided by a nurse anesthetist. Private nurses are allowed to work outside hospitals if they have a general license. The only requirement is to declare once a year the money they receive.
The situation is quite different in Georgia that inherited the inefficient Semashko system from the Soviet Union like Ukraine and began the reform process to introduce a health insurance system a few years ago. Like in Ukraine, nursing personnel in Georgia did not receive enough attention during the reform’s development. This led to a critical lack of nurse staff. Georgia has far fewer nurses than doctors, with some of them being student doctors that will later occupy doctor positions. For comparison, in the countries of the Organization for Economic Cooperation and Development, on average there are three nurses to every doctor.
Georgia has completely gotten rid of the Soviet system of further education courses but offered nothing in exchange. The professional development of nurses is not regulated at the state level depending entirely on the practices of a particular hospital.
Due to low wages, nurses often combine work in several medical institutions. The regulator does not like this as it can cause fatigue and reduce the nurses’ quality of work. The Ministry plans on keeping a close watch of the register and prohibit such combining. However, this will not solve the problem as the reason for this practice is low wages. It is therefore not surprising that many nurses emigrate from Georgia to the EU, where they are offered decent working conditions and residence permits for their families.
If Ukraine does not pay attention and empower nurse personnel, it has the chance to face problems like those faced by Georgia.
What did our study show?
In 2021, as part of the project “Creation of the Roadmap for nursing development in Ukraine” with the support of the International Renaissance Foundation, the VoxUkraine and the Center for Nursing Development of the Ministry of Health of Ukraine teams conducted 19 interviews and desk research studying the nursing services systems of Ukraine and selected countries (the United States, the UK, Georgia). During the study, we identified the following issues inherent in Ukraine’s system of nursing services:
- low wages are the main reason for dissatisfaction with the job of the nurses we surveyed. The nurses’ salary rarely exceeds the minimum wage set by the Government. Research into the reformed primary care conducted in 2019 also did not show any significant increase in the salaries of nurses. The interviewed nurses said that it would be fair if their salary were UAH 10-15 thousand.
- professional secondariness. The respondents view nurses as doctors’ assistants, even when they admit that a nurse sometimes does perform the work of a doctor. This is partly due to traditional attitudes and to legislative regulations (de jure) that do not allow nurses to perform medical procedures and prescriptions without the approval of a doctor. At the same time, both doctors and nurses see opportunities for increasing nurses’ independence, especially given the possibility of obtaining higher education. Therefore, the education system is already ready to empower nurses. But is the labor market ready?
- The educational content does not meet workplace requirements. One of the reasons is that nurses having practical experience are still not very often involved with teaching in medical colleges. The teaching of medical subjects is mainly done by doctors who only see the “outer” side of nurses’ work and are not familiar with all modern trends in nursing.
“I graduated from a medical college myself and I remember what we were taught there. And we weren’t taught how to talk to patients, how to tell bad news. We learned that in a hospital chamber,” a hospital director said.
“In colleges, they tell you a lot of useful things, but when it comes to working, they speak generally, without telling everything. For instance, I had this subject, “Patient Care”, where we learned how to fill out patients’ cards, temperature sheets and so on. When I came to work here (I had an internship), I saw that the documents were filled out in a totally different way. The teachers teach the way they learned themselves, but they are theorists, not practitioners,” a nurse said.
- The outdated system of in-service training. Further education courses taking place every 5 years mostly perform a formal function providing outdated information. Like the medical profession, nursing requires continuous training (obtaining a certain number of points each year). Such trainings will be launched at 2023. Another problem of obtaining qualifications is their “zeroing out” in the case of changing specialty.
“I have 22 years of experience. For over ten years, I’ve had the highest category. And now that I’ve switched to work [in another specialty], I realized that I was losing all my categories. I’ve got to start all over again, working here for 2 or 3 years. Will there ever be a law allowing the nurses who spend years earning these categories to not lose them when changing jobs?” a nurse said.
- The lack of involvement in decision-making at the level of hospitals and government bodies. Currently, this depends on the goodwill of the hospital management and the authorities. Nurses do not see tools that could guarantee that their voices will be heard. General meetings do not have such a function because hospital heads often can make key decisions on their own. The interviewed nurses are interested in the opportunity to join working groups at government bodies to present their position.
“It would be very good if they engaged nurses to participate in such [working] groups to see all this work from the bottom up,” a nurse said.
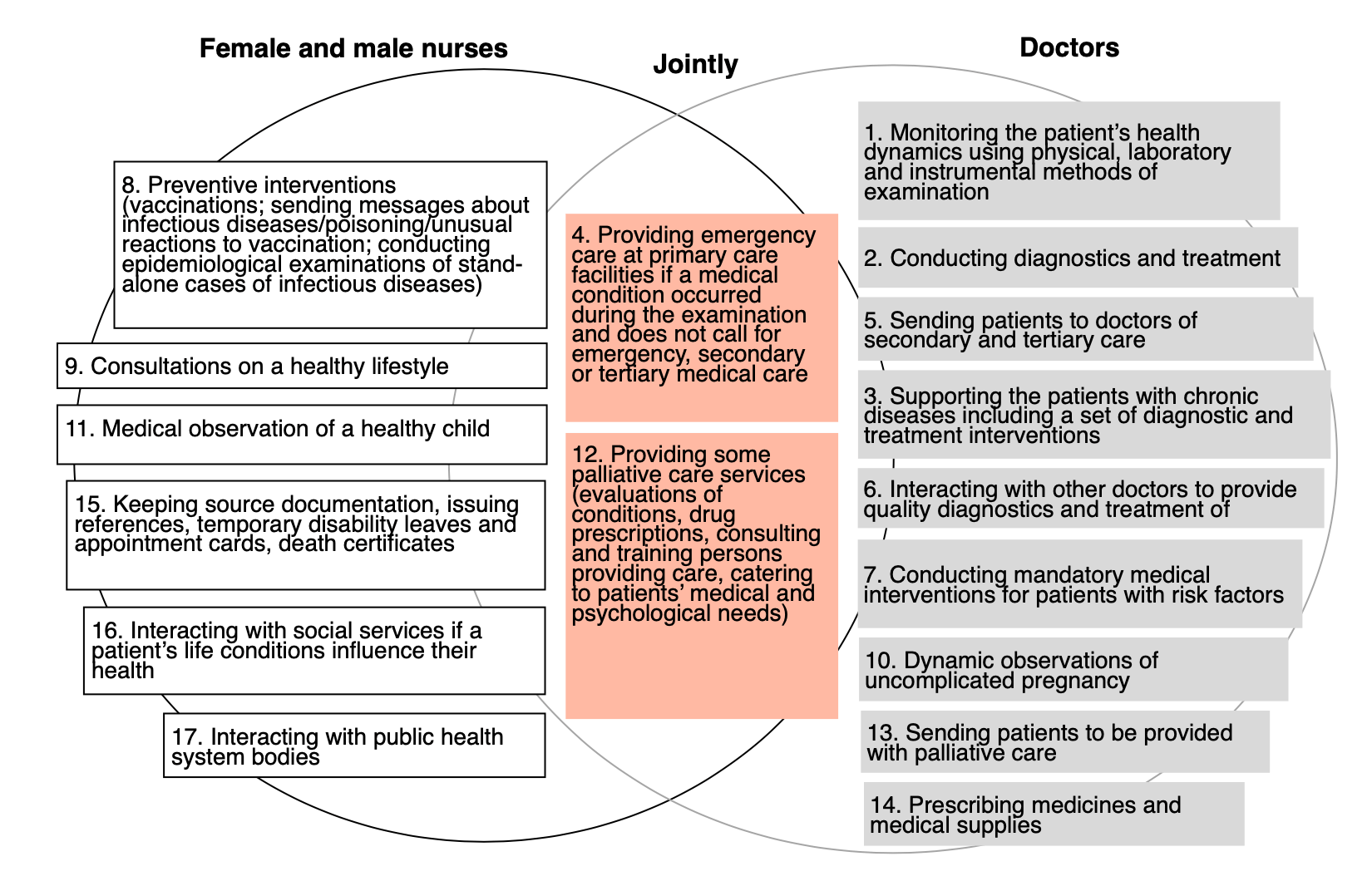
- The absence of separate funding for nurse (midwife) services from the NHSU. Many of the services listed in the NHSU packages are provided by mid-level medical staff (Figure 1). However, the lack of separate funding for nursing services leads to a conflict of interest between doctors and nurses and paramedics because they view for a limited amount of funds.
If we use the package of medical services provided by a family doctor as an example, an increase in nurses’ wages means a decrease in family physicians’ income. This problem is especially noticeable in rural areas, where one family doctor maintains an ambulatory care clinic and feldsher-midwife stations using the money received from the declarations. This puts the doctors at a disadvantage compared to their urban counterparts as well as makes it difficult for ATCs to find family doctors. When such doctors move to a city where they do not need to support the FMSs at their own expense, then the FMSs should be closed down as was the case in the villages of the former Vesele hromada.
Figure 1. Distribution of services between doctors and nurses in the family doctor’s package of services
Data source: MOH Order No.504 On the Procedure for the Provision of Primary Health Care
NB: The graph contains abbreviated names, whose full versions can be found in the Ministry of Health’s Order No.504. It should be noted that a part of the services attributed by us to doctors are already provided by nurses in the UK, including uncomplicated pregnancy care and issuing prescriptions for drugs and medical supplies. Besides, in the United Kingdom and the United States, palliative care is provided mainly by nurses. Therefore, this distribution needs to be revisited from time to time.
- The officially registered private practice is not widespread. Although nurses have the opportunity to officially register as private practitioners, not many of them use it. Among the reasons are being unaware of the possibility, a lack of steady demand for private services (i.e. nurses provide such services unofficially and from time to time), legal and financial knowledge, as well as the money to pay for legal advice and accountants, office equipment, and for advertising their services.
“She has a formal salary, works in a formal medical facility, and [has] very little [free time]. On days when the nurse is free, she has to visit someone’s home, perform medical procedures and get the money. Such requests are very rare, but if there is such a thing, then it’s a very good side job,” a nurse said.
“I worked alone. An hour of my work is from 300 hryvnias. For example, I visited people at home, the doctor prescribed a person to drip drugs, and so I dripped them. I do this procedure, I put a catheter in or the Venflon, I drip, I monitor the patient’s condition, and after I’ve done that, I’m free,” a nurse said.
All these problems eventually lead to a drop in the popularity of the nursing profession and a decrease in the number of nurses. According to data from the Center for Health Statistics of the Ministry of Health of Ukraine, there were 262,000 nurses in Ukraine in 2015, but 5 years later, in 2020, their number decreased to 213.4 thousand. This limits Ukrainians’ access to medical services because nurses spend much of their time around patients. They often serve as “patients’ entry point” to a medical institution, so it is not surprising that patients trust nurses even a little more than doctors in Ukraine* (66% and 63%, respectively).
Recommendations
We offer some recommendations that should help resolve the above problems and revive the attractiveness of the nursing profession.
Outlining a clear sphere of activity and responsibility of nurses, with separate funding. After receiving prescriptions and treatment regimens from a physician, the need for nursing services is often the only reason for the patients to stay in the hospital. After all, not everyone has the opportunity to visit their family doctor to get daily injections or infusions, both for logistical reasons (the patient’s condition, a lack of regular transport connections in the villages, etc.) and because of the doctor’s workload. The responsibilities of family doctors include visiting their patients. This service is especially relevant for the elderly and patients living in remote villages. But there is usually no such practice, as well as no social transport that could take villagers to their doctor if need be.
Having a separate package of nursing services – “Nursing care for adults and children” – under the medical guarantees program, provided outside of the hospital and based on a doctor’s prescription (including for postoperative recovery, palliative care, preventive measures), would improve the patients’ access to medical services. It would also reduce the financial pressure on family doctors, as it would mean that the services provided by FMSs (or independent nurses performing similar functions) could be funded not from a family doctor’s “pocket”, but by a separate NHSU package.
Streamlining educational opportunities for nurses. Like doctors, nurses will get a system of continuous professional development. According to Decree No.725 by the Cabinet of Ministers of July 17, 2021, this opportunity will be available for them as of January 1, 2023. Another way of improving the quality of the acquired knowledge and skills can be the introduction of a dual education programs. A dual programs for nurses will allow them to immediately apply their knowledge in practice and be paid for it, providing health care facilities with additional nursing personnel. At the beginning of their training, nurses can work as junior nurses (nursing assistants) because this position does not require medical training, and, when the level of their knowledge grows, occupy the positions of regular nurses.
Improving access to health services by empowering nurses and extending private nurse practice. Ukraine is not the first country in the world to face the high cost of medical services and limited access to them. Making the family physician a key person in accessing medical services (gatekeeper) for the patient, health care reform left out the residents of hromadas faced with an acute shortage of family doctors. Even the most experienced doctors are not able to have enough time to provide quality medical services to all those who signed a declaration with them. If a doctor works 11 months a year (i.e. about 48 weeks excluding vacation, sick leaves, etc.) 33 hours a week, then she/he has a little less than 1,600 working hours. With a recommended number of declarations – 1800 – this means 53 minutes per patient per year. Quite obviously, the doctor will not have enough time to dedicate to preventive measures, including periodic examinations of patients at risk, focusing instead on the treatment of patients. This number of working hours is also unlikely to be enough to visit patients at home, even if they need it.
The British experience shows that empowering nurses has improved the patients’ access to health care, and the prescriptions written by nurses work even better than those prescribed by doctors (according to assessments of the condition of patients that took medication). The respondents noted that nurses with higher education already have enough knowledge to perform some of the doctors’ functions, and the representative of an educational institution stressed that the educational system is able to provide nurses with knowledge and skills to embrace greater responsibility.
To encourage nurses to take on more powers, decent compensation for their work needs to be provided. Here, private practice can come in handy and be combined with the main job (or be done separately) giving more opportunities to influence your earnings. A variety of training programs, as well as the free advice service on how to start your own business from the regulator, can help promote the practice of starting a private nursing business.
Conclusion
Structuring and expanding the responsibilities of nurses, introducing separate funding for nursing services and making private nursing practice commonplace would fix the most glaring problems in this area, i.e. viewing nurses only as doctors’ assistants, and low wages of the mid-level health care staff.
These problems are closely related to all other problems. Low wages and habitual perceptions of nurses in the hospital environment as ancillary staff robs them of self-confidence, limits their desire to develop, leaves them vulnerable to everyday life problems and creates a big temptation to obtain informal payments from patients. And the lack of funds to start their own business (training, equipment, licensing, legal and accounting services) hinders the spread of private nursing practice that would facilitate access to medical services for Ukrainians and enable nurses to improve their financial situation and achieve greater independence.
Attention
The authors do not work for, consult to, own shares in or receive funding from any company or organization that would benefit from this article, and have no relevant affiliations