How has the ongoing war reshaped healthcare in Ukraine beyond the immediate devastation? This question lies at the heart of understanding the complex dynamics of informal payments within the healthcare system – a persistent challenge exacerbated by the full-scale war. Amidst the turmoil, can effective policy interventions help mitigate the financial burdens these payments impose on patients, particularly during such critical times?
This work investigates the dynamics of these payments in a war-affected setting, analyzing how the armed conflict has influenced the prevalence and magnitude of informal payments. Interestingly, despite the chaos, 2023 witnessed a decline in such payments compared to the pre-war era, possibly reflecting the compounded effects of economic strife and healthcare disruptions.
Why do informal payments (henceforth IPs) in healthcare persist, and how do they affect the daily lives of ordinary Ukrainians? In recent years, according to the World Health Organization, IPs for healthcare services have emerged as a significant concern across various nations, with Ukraine being no exception. IPs deepen inequalities, restrict access to necessary medical care, and disproportionately burden those least able to pay. With the outbreak of the full-scale war on February 24, 2022, these challenges have only intensified, further straining the healthcare system crippled by economic and infrastructural disruptions. This study aims to delve into the dynamics of IPs for health care services in Ukraine, focusing on the influence of war and other relevant factors on their prevalence and magnitude.
How does war impact informal payments in healthcare?
The importance of this study stems from its examination of the specific circumstances of a nation engaged in war. While prior research has addressed informal payments in peace settings, there is a notable gap in the literature regarding their dynamics within war-affected environments. This research is crucial for both scholarly inquiry and policy-making, as it aims to shed light on how the war influences healthcare funding and access, thereby guiding strategies to alleviate the negative impacts of IPs on at-risk groups.
My study looks into how the full-scale war affected the frequency of informal payments in healthcare and their size. Apriori the effect is not known: reduced incomes of people may reduce both instances and size of informal payments while lower supply of healthcare services due to destruction of facilities and mobilization of medical workers may increase IPs.
Thus, I look at the number of factors – regions where a person lives, his/her income, attitude to informal payments and a number of demographic characteristics.
Data description
The data for this analysis were collected through two anonymous patient surveys conducted within medical institutions across Ukraine. Initially, the dataset included 4079 observations, but after removing records that did not have answers to the main questions, we were left with 3795 observations. These surveys were part of studies conducted in 2019-2020 and 2022-2023 by USAID Health Reform Support and KSE Institute and focused on four key healthcare services: medical care during childbirth, care for newborns in complex neonatal cases, care for acute myocardial infarction, and acute cerebral stroke. The surveys included responses from patients and their families who received care in urban and rural areas. The data collected included a range of factors:
- Variables of interest: amount of informal payments and the likelihood of making these payments.
- Demographic: age, gender, education level, settlement type (urban or rural), and employment status.
- Geographic: residence in different macroregions of Ukraine and war-affected territories.
- Socio-Economic: household income levels and vulnerability categories (these included social and health vulnerabilities).
- Attitudinal: attitudes towards informal payments and whether payments were made by hint, request, coercion or voluntarily.
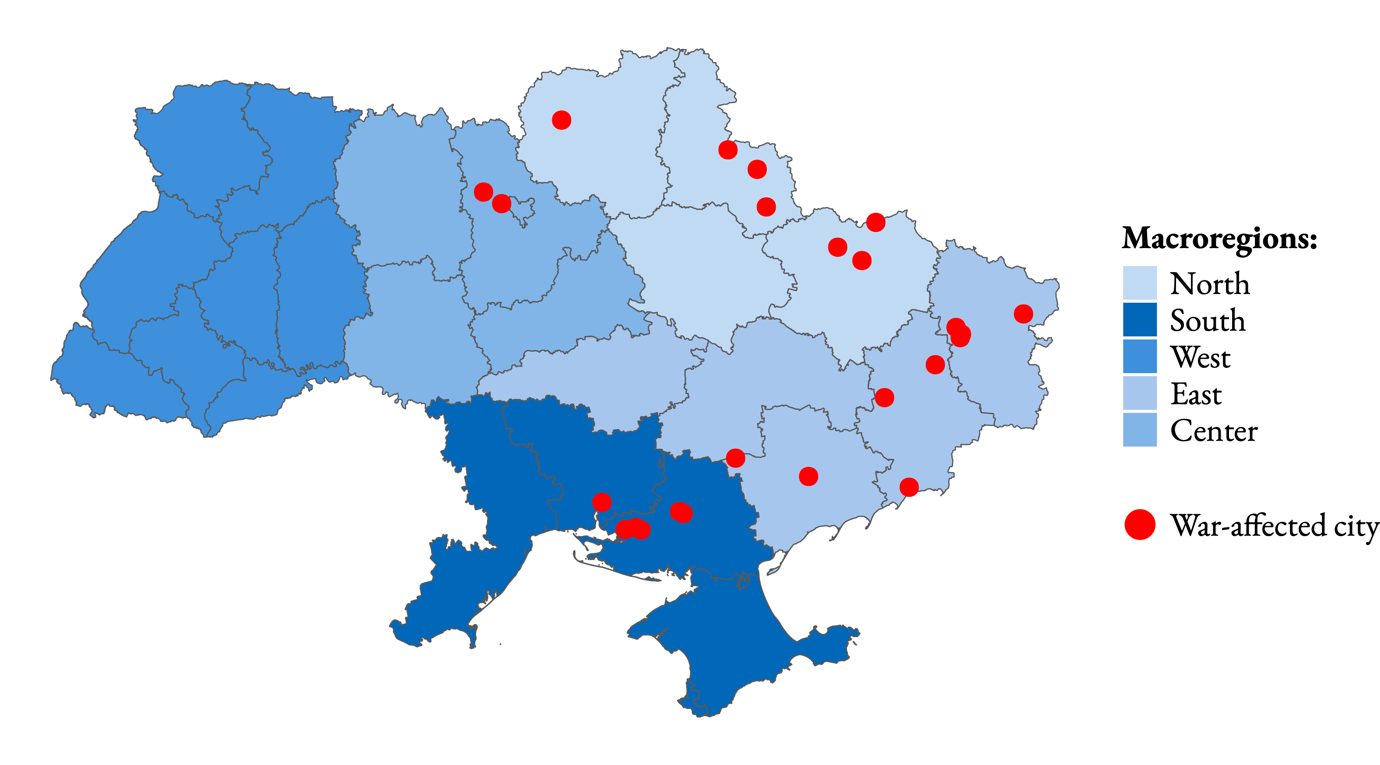
Territories directly affected by the ground-level attack include settlements in Kyiv, Sumy, Chernihiv, Donetsk, Luhansk, Kharkiv, Zaporizhzhia, Kherson, and Mykolaiv regions that experienced ground-level attacks since February 24, 2022 and are shown in Figure 1.
Figure 1. Geography of the data
Note: the geographic distribution according to the USAID HRS and KSE Institute study
These settlements, identified by respondents as their places of residence, are situated in close proximity (up to 10 kilometers) to the hostilities or directly at the epicenter. The classification is done via DeepStateMap and includes settlements such as Kharkiv, Vovchansk, Chuguyiv, Mariupol, Bakhmut, Tokmak, Kamyyanka-Dniprovska, Sumy, Trostianets, Chernihiv, Novotroitske, Mykolaiv, Kherson, Oleshki, Beryslav, Kakhovka, Irpin, Borodianka, Bilopilla, Severodonetsk, Bilozerka, Lysychansk, Rubizhne, and Bilovodsk. The survey was implemented in all of these cities. In total 18% of respondents belonged to war-affected areas.
85% of our respondents live in urban areas, 52% have higher education and 76% are female (this reflects the fact that two of the four studied services were related to childbearing and neonatal care and also to the fact that women in general are more likely to visit doctors). Average age of respondents is 46 years, while age distribution has two peaks: 22-34 years and 66-74 years (again related to services for which the data was collected).
65% of respondents had a negative attitude to informal payments, while 26% had a neutral attitude and 9% – positive attitude. 48% of respondents made IP by hint, request or coercion, while for others this was a voluntary act.
The main results
The findings reveal a significant decline in the likelihood and magnitude of informal payments in 2023 compared to the pre-war period. The likelihood of informal payments in 2023 was 10.5 p.p. lower than in 2020, and the magnitude of informal payments in 2023 was 86.8% lower than in 2020 (in 2023 prices).
Regions close to the frontline were not different from other regions in terms of probability of informal payments (i.e. there, the decline in probability was the same as elsewhere – about 10 p.p.). However, the reduction of informal payments there was significantly smaller than in other regions – by 40-50% in different specifications. This suggests that reduced supply of healthcare services in those regions plays a more important role than elsewhere – probably because it was more severe near the frontlines.
Other factors that significantly impacted informal payments were as follows. In all the macroregions the probability of informal payments was lower than in the Central region (from about 3 p.p. in the East to 9-10 p.p. in North and West), and for the size of the payments only the Western region was significant: there, IPs are on average 17-20% lower, than in the Central region. This result may be due to the fact that the Central region includes Kyiv city, where people have higher ability to pay and some unique (or better quality) healthcare services may be offered.
Demographic characteristics are insignificant: age slightly decreases the probability and increases magnitude of IP but the effect is very small.
However, people from urban areas and those who are employed make significantly higher informal payments (by about 27% and 13% respectively), although these factors do not affect the probability of payments. People from socially vulnerable groups have lower probability to make informal payments (probably because they are less able to do that), while people with health vulnerability tend to make higher informal payments (probably due to their health needs). Positive attitude towards IP increases probability of informal payment (by 6 p.p.) but not its size, while the fact that IP was made by hint, request or coercion increases both its probability (by 20 p.p.) and size (by 40%).
Conclusions
The war has significantly affected informal payments in Ukrainian healthcare. On the supply side, lower availability of healthcare facilities may increase the incentives of medical workers to ask for informal payments. On the demand side, the need for healthcare services probably increased but the ability to make informal payments likely declined as people became poorer. We find that the second effect is larger, since both probability and size of informal payments declined in 2023 compared to 2020. At the same time, the decline in their size was lower in areas more affected by war, which is probably a reflection of higher scarcity of healthcare provision there.
Demographic and socio-economic factors, including income levels and employment status, showed little influence on the likelihood or amount of informal payments. This suggests that informal payments are a systemic issue, influenced more by overarching cultural norms and systemic healthcare deficiencies than by individual economic conditions. Therefore, reduction of informal payments requires a comprehensive public policy. Such policies have been introduced in Ukraine since 2017 within the healthcare reform (proper “sorting” of patients with family doctors as gatekeepers, more competition and higher standards of healthcare services, “money follows a patient” framework) but more can be done:
Public awareness campaigns. Educating people about the illegality and harmful effects of informal payments is essential. This can be done via broad media campaigns using different types of “traditional” and social media. Community engagement initiatives such as organizing meetings and workshops can help educate people on the ground. Incorporating lessons on patients’ rights and anti-corruption practices into school curricula can foster transparency and accountability culture.
Enhancing patient feedback mechanisms. Establishing robust systems for patient feedback and grievances is crucial. This can include setting up anonymous hotlines for patients to report instances of informal payments and other issues, creating online portals where patients can submit feedback and complaints, and ensuring that reported cases are investigated with appropriate actions taken against offenders. These measures will help identify problematic areas, hold providers accountable, and ultimately reduce the prevalence of informal payments.
By implementing these specific measures, alongside increased funding and stronger regulations, Ukraine can work towards significantly reducing informal payments in the healthcare system. This will not only improve equitable access to medical services but also enhance the overall quality of healthcare for its citizens, even amidst the ongoing war.
Attention
The author doesn`t work for, consult to, own shares in or receive funding from any company or organization that would benefit from this article, and have no relevant affiliations