In the third year of the full-scale aggression Ukrainians still rely on public health care with 48.3% of households reporting visits to public medical facilities over the last 12 months. However, corruption continues to hinder equitable access, with 16.9% of these households making unofficial payments or offering gifts while using public healthcare.
Although this level of informal payments seems substantial, it is still much less than 30.8% reported in 2016 let alone 43.8% reported in 2010. War-related violence has further exacerbated the challenges of public healthcare, and 15.7% of respondents faced difficulties accessing healthcare services due to damaged facilities or the unavailability of medical personnel.
War and healthcare
After the start of the full-scale aggression in 2022 Ukraine has been facing significant challenges along many dimensions of life including the healthcare system. The catastrophic consequences of conflict for healthcare systems have been the subject of extensive academic research. Wars often exacerbate pre-existing inequalities, disrupt infrastructure, and challenge the resilience of public health institutions. Drawing on contemporary academic sources, this review explores these dynamics, with Ukraine serving as a poignant case study.
Wars severely disrupt healthcare systems, exacerbating vulnerabilities and creating complex challenges for service delivery, workforce stability, and patient care. Damaged facilities and displaced personnel often leave healthcare systems operating at a fraction of their capacity. For instance, during the conflict in Tigray, Ethiopia, less than a third of hospitals were functional, echoing similar challenges faced in Ukraine where damaged infrastructure and systemic corruption hinder equitable healthcare access (Gesesew et al., 2021; Mueller et al., 2024).
Healthcare workers become pivotal in war zones, addressing immediate medical needs while facing significant psychological tolls. They play essential roles in advocating for systemic recovery, and international collaboration is crucial to ensure their safety and effectiveness (Kumar & Kamath, 2024). These challenges are amplified when conflicts coincide with other crises, such as the COVID-19 pandemic, which compounded the strain on healthcare systems in Tigray, resulting in steep declines in patient visits and access to care (Abraha et al., 2023).
Economic inequality and corruption further compound the difficulties in accessing healthcare during conflicts. Prevalence of informal payments and inequities may exacerbate existing barriers and disproportionately affect vulnerable populations. Additionally, post-conflict mental health burdens, particularly post-traumatic stress disorder (PTSD), significantly increase long-term healthcare expenditures, emphasizing the need for mental health services in recovery frameworks (Sabes-Figuera et al., 2012).
Coordinated medical evacuation efforts have proven vital in mitigating war’s impact on healthcare. In Ukraine, such efforts successfully transported critically ill patients, particularly those with trauma or life-threatening conditions, demonstrating the effectiveness of international cooperation in addressing health crises (Mueller et al., 2024). Furthermore, addressing the psychological scars of conflict is crucial, as unaddressed mental health issues hinder societal recovery and long-term resilience (Sabes-Figuera et al., 2012).
The challenges faced by healthcare systems in conflict zones underscore the need for robust international strategies, resilient local infrastructures, and comprehensive recovery plans. The Ukrainian experience reflects a broader global pattern where war undermines healthcare equity and accessibility, calling for concerted efforts to rebuild and reform these systems (Gesesew et al., 2021; Mueller et al., 2024; Kumar & Kamath, 2024).
Public healthcare and violence during the war
To address the issues raised in this article we commissioned questions to be added to the December 2024 Omnibus survey by Kyiv International Institute of Sociology (KIIS) that provides a detailed portrait of the socio-economic and demographic characteristics of 2,000 respondents in Ukraine, in particular related to their experience with using public health care and war-induced challenges. Survey weights were used to compensate for deviations from official statistical data (based on State Statistics Service as of January 1, 2021), thus, offering a comprehensive view of national trends.
Sample description
Socio-demographic and socio-economic characteristics of the sample show the complex structure of respondents remaining in Ukraine. The survey reveals that the average age of respondents is 47.9 years, with a slight female majority at 54.7%. In terms of urbanization, a diverse range of settlement sizes is represented with villages being a base category. A small proportion of respondents, 4.2%, live in settlements with populations under 20,000, while 4.9% reside in medium-sized cities with populations between 20,000 and 49,000. Cities with 50,000 to 99,000 inhabitants account for 4.7% of respondents. 22.8% live in large cities with populations ranging from 100,000 to 499,000 and 26.9%, reside in very large cities with populations exceeding 500,000. 44.7% of participants live in regional (oblast) centers. In terms of regional representation, 28.9% of respondents are from Western Ukraine, 23.5% from the South, and 10.0% from the East while the rest live in the Center (base category).
Educational attainment among respondents varies widely as well with high school diploma or less being a base category. In particular, 5.6% completed vocational school and 34.7% attended technical school. A significant proportion, 39.7%, have higher education degrees while 3.9% of the sample has incomplete higher education.
Employment status reflects a diverse spectrum of the population starting with unskilled workers as a base category. Among the respondents, 6.6% are employees without higher education, while 21.0% are professionals with higher education. Self-employed individuals account for 4.6%, entrepreneurs 4.5%, and those in military service 2.7%. Meanwhile, 7.4% are househusbands or housewives, 29.0% are retirees, 3.8% are students, and 4.8% are unemployed.
Healthcare access and systemic challenges remain pressing issues as Table 1 indicates. Over the past year, 48.3% of households reported seeking medical assistance within the public healthcare system. However, corruption continues to hinder equitable access, with 16.9% of these households making unofficial payments or offering gifts while using public healthcare. While this level of informal payments seems substantial, it is still much less than 30.8% in 2016 and even 43.8% in 2010 reported in our previous VoxUkraine article based on “Life in Transition” Surveys II and III. 15.7% of respondents faced difficulties accessing healthcare services due to damaged facilities or the unavailability of medical personnel.
The ongoing war has profoundly affected daily life in Ukraine. Since February 24, 2022, 20.3% of respondents have suffered property damage, while 20.0% have sustained injuries or death of relatives or loved ones. Additionally, 12.1% faced major inconveniences, including life-threatening shortages of essential resources like food and medical assistance, while 30.2% dealt with minor inconveniences such as power outages or the unavailability of necessary goods. Moreover, 12.6% have become internally displaced persons. But even before the full-scale aggression, 3.1% had experienced war-related violence brought by Russia to Crimea and Donbas.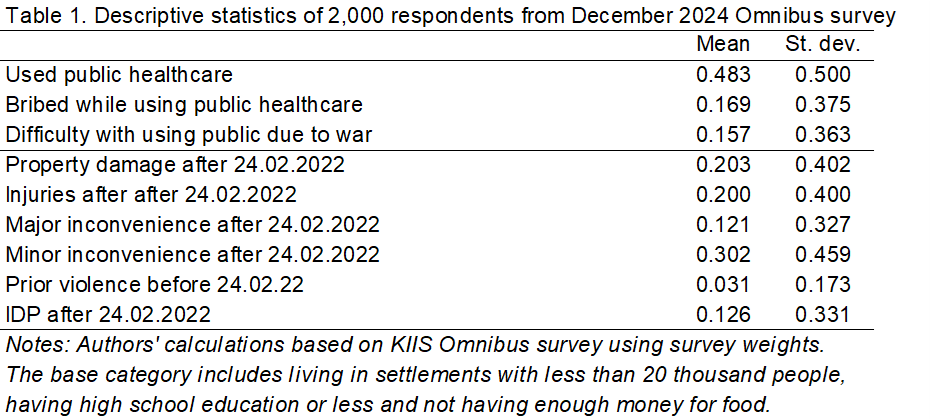
The economic circumstances of the respondents paint a stark picture of the war-related challenges: 34.0% report having sufficient funds only for food, while 35.9% can afford food and clothing. A smaller group, 15.0%, can purchase some expensive items, and only 2.5% feel they can afford anything they desire. The remaining base category of respondents not having enough money for food represents 12.6%.
These results highlight the severe socio-economic and psychological toll of the war, compounded by persistent systemic corruption and inadequate infrastructure further threatened by the war.
Factors affecting public healthcare use during the full-scale war
The linear probability models presented in Table A1 in the Appendix estimate the effects of violence and other factors on public healthcare use, informal payments within those public healthcare settings, and difficulties accessing public healthcare due to war. The base category includes households that didn’t use public health care but could have visited a private provider, a pharmacy, a traditional healer or none of those. Linear probability models are estimated using ordinary least squares with survey weights, robust standard errors and clustering at the level of region (oblast).
Somewhat surprisingly, not all types of violence translate into tangible effects on public healthcare use, perhaps, due to widespread effects of a barbaric russian aggression. In particular, individuals who experienced property damage after February 24, 2022, are significantly more likely to face difficulties accessing public healthcare services by 17.8% (p<0.01). This result is probably expected given that some regions suffered more from war-related damages of private dwellings as well as public facilities.
Experiencing minor inconveniences after February 24, 2022, is associated with increased probability of using public healthcare by 5.8% (p<0.05), making an informal payment or gift when using public healthcare by 6.6% (p<0.05), and facing difficulties with accessing public healthcare due to war by 9.8% (p<0.01). Prior experiences of violence before February 24, 2022 is associated with 11.3% lower probability of making an unofficial payment or gift.
Respondents who became internally displaced persons (IDPs) after the escalation of the war in February of 2022 are less likely by 7.7% to report difficulties with accessing public healthcare due to absence of personnel or destroyed healthcare infrastructure (p<0.01), potentially reflecting the effect of relocation from war-affected zones to less affected areas.
The likelihood of using public healthcare services appears also to be influenced by socio-economic and demographic factors. For instance, individuals with higher education are significantly more likely to use public healthcare by 13.4% (p<0.01). Similarly, those residing in oblast centres have higher probabilities of using public healthcare by 10.8% potentially showing easier access via public transport (p<0.05).
Bribery in healthcare is another pressing concern. Military service members are less likely to report engaging in bribery by 18.1% (p<0.05), while those with vocational education are similarly less prone to bribery by 12.7% (p<0.05) compared to a base category of having a high school diploma. On the other hand, entrepreneurs are more likely to report paying bribes or offering gifts within the healthcare system by 21.6% (p<0.10) compared to a base category of manual workers, underscoring persistent inequalities in access. IDPs are also less likely to report informal payment by 7.8% points (p<0.10) which may indicate either their lack of funds or preferential treatment by healthcare providers who may be aware of a patient’s IDP status.
Economic conditions further shape healthcare dynamics. Individuals with sufficient funds for food and clothing are more likely to use public healthcare by 8.0% (p<0.10) and are less likely by 5.1% (p<0.10) to have difficulties with accessing public healthcare due to the full-scale war. At the same time, a small group of those who can afford some expensive items are also less likely to face difficulties accessing services by 6.4% (p<0.10). These findings highlight the intertwined effects of socio-economic status on healthcare access.
Overall, the analysis underscores how the war has exacerbated systemic challenges within Ukraine’s healthcare system. War-related property damage and inconveniences have a clear impact on access to services, while socio-economic disparities and corruption continue to shape healthcare utilization and equity. These results call for targeted interventions to address these pressing issues and ensure more equitable access to healthcare amidst ongoing conflict.
Conclusions
Despite the ongoing war nearly half of Ukrainian households (48.3%) visited public medical facilities in the past year, reflecting the resilience of public healthcare services. In addition, the rate of informal payments in public healthcare has significantly declined—from 43.8% in 2010 to 16.9% in 2024 — indicating gradual progress in reducing corruption. However, the war context poses major challenges with access because 15.7% of respondents reported difficulties accessing care due to damaged facilities or the absence of medical personnel.
The dual burden of war and structural inefficiencies underscores the need for targeted reforms in public health care. Addressing these challenges will require significant efforts to rebuild infrastructure, eradicate corruption, and ensure equitable access to essential health services for all Ukrainians. Despite the war hardships, the resilience of the Ukrainian public health care system remains evident. However, the path to recovery and reform will demand a concerted effort from both domestic and international stakeholders. It is also an utmost priority to continue monitoring changes in access to public healthcare as well as the extent of informal payments.
Specifically, the government and its international partners should prioritize anti-corruption initiatives that strengthen oversight, transparency, and accountability within public healthcare. Investments in rebuilding and modernizing medical infrastructure — particularly in conflict-affected areas – must be accompanied by efforts to attract healthcare workers to ensure dependable service provision. Empowering local communities, raising public awareness about patients’ rights, and improving reporting of corruption cases can further reduce bribery risks and foster equitable healthcare access for all Ukrainians in the country torn by brutal russian aggression.
References
- Kumar YS, Kamath JS. Healthcare Workers on the Frontlines of War: Essential Roles and Responsibilities. Am J Med Open. 2024;11:100064.
- Mueller A, Salek M, Oszer A, et al. Retrospective comparative analysis of two medical evacuation systems for Ukrainian patients affected by war. Eur J Cancer. 2024;210:114271.
- Gesesew H, Berhane K, Siraj ES, et al. The impact of war on the health system of the Tigray region in Ethiopia: an assessment. BMJ Glob Health. 2021;6(11):e007328.
- Sabes-Figuera R, McCrone P, Bogic M, et al. Long-term impact of war on healthcare costs: an eight-country study. PLoS One. 2012;7(1):e29603.
- Abraha HE, Tequare MH, Teka H, et al. Impact of a double catastrophe, war and COVID-19, on health service utilization of a tertiary care hospital in Tigray. Confl Health. 2023;17(1):37.
- Ventevogel P, Jordans M, et al. Post-conflict mental health services: A systematic review. Int J Ment Health Syst. 2015.
Appendix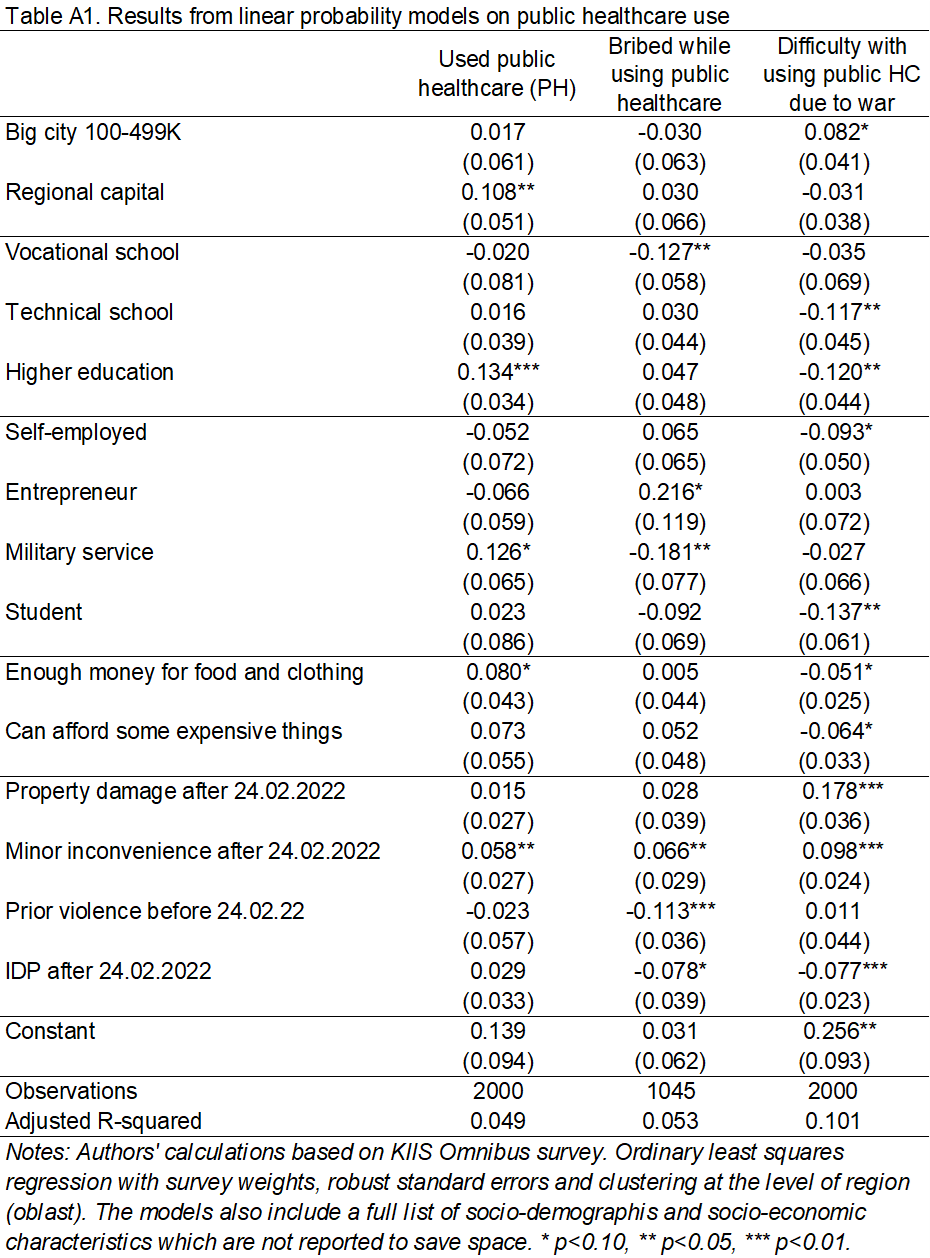
Photo: depositphotos.com/ua
Attention
The authors do not work for, consult to, own shares in or receive funding from any company or organization that would benefit from this article, and have no relevant affiliations